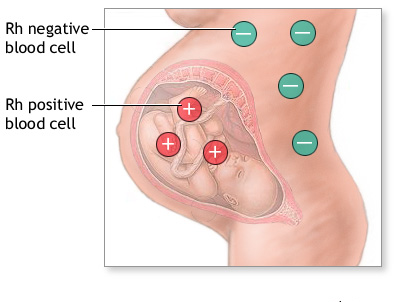
During pregnancy, problems can occur if a woman blood group is Rhesus Negative and her foetus is Rhesus Positive. Rhesus us shortly written as Rh.
From Wikipedia Rh (D) disease, rhesus incompatibility, Rhesus disease, RhD hemolytic disease of the newborn, rhesus D hemolytic disease of the newborn or RhD HDN) is a type of hemolytic disease of the newborn (HDN). The disease ranges from mild to severe, and typically occurs only in some second or subsequent pregnancies of Rh negative women where the fetus’s father is Rh positive, leading to a Rh+ pregnancy. During birth, the mother may be exposed to the infant’s blood, and this causes the development of antibodies, which may affect the health of subsequent Rh+ pregnancies.
In mild cases, the fetus may have mild anaemia with reticulocytosis. In moderate or severe cases the foetus may have a more marked anaemia and erythroblastosis fetalis (hemolytic disease of the newborn). When the disease is very severe it may cause hydrops fetalis or stillbirth.
Rh disease is generally preventable by treating the mother during pregnancy or soon after delivery with an intramuscular injection of anti-RhD immunoglobulin (Rho (D) immune globulin). The RhD protein is coded by the RHD
Effects of different Rh of baby and mother
- Miscarriage
- Abortion
- Ectopic pregnancy — when a fertilized eggs implants somewhere outside the uterus, usually in a fallopian tube
- Molar pregnancy — a noncancerous (benign) tumor that develops in the uterus
- Amniocentesis — a prenatal test in which a sample of the fluid that surrounds and protects a baby in the uterus (amniotic fluid) is removed for testing or treatment
- Chorionic villus sampling — a prenatal test in which a sample of the wispy projections that make up most of the placenta (chorionic villi) is removed for testing
- Bleeding during pregnancy
- Blunt trauma to the abdomen during pregnancy
- Rotation of a baby in a breech position — such as buttocks first — before labor
- Fetal blood sampling
Rh factor blood test
Rhesus (Rh) factor is an inherited protein found on the surface of red blood cells. If your blood has the protein, you’re Rh positive. If your blood lacks the protein, you’re Rh negative.
Rh positive is the most common blood type. Having an Rh negative blood type is not an illness and usually does not affect your health. However, it can affect your pregnancy. Your pregnancy needs special care if you’re Rh negative and your baby’s father is Rh positive.
Your health care provider will recommend an Rh factor test during your first prenatal visit. This test will identify your blood type and whether your blood cells carry the Rh factor protein.
Why it’s done
The Rh factor test is done during pregnancy to identify a woman’s Rh factor. In some cases, the baby’s father might need an Rh factor test, too.
During pregnancy, problems can occur if you’re Rh negative and the baby you’re carrying is Rh positive. Usually, your blood does not mix with your baby’s blood during pregnancy. However, during delivery or certain times during pregnancy, a small amount of your baby’s blood could come in contact with your blood.
If you’re Rh positive, Rh incompatibility isn’t a concern. If you’re Rh negative and your baby is Rh positive, however, your body might produce proteins called Rh antibodies after exposure to the baby’s red blood cells. The antibodies produced aren’t a problem during the first pregnancy. The concern is with your next pregnancy. If your next baby is Rh positive again, your body will produce Rh antibodies that can cross the placenta and damage the baby’s red blood cells. This could lead to life-threatening anemia, a condition in which there are not enough red blood cells. If this condition is not prevented, each Rh positive baby you carry after your first pregnancy might have severe anemia.
If you’re Rh negative, you might need to have another blood test — an antibody screen — during your first trimester and again during week 28 of pregnancy. The antibody screen is used to detect antibodies to Rh positive blood.
If you haven’t started to produce Rh antibodies, you’ll need an injection of a blood product called Rh immune globulin. The immune globulin prevents your body from producing Rh antibodies during your pregnancy.
If your baby is born Rh negative, no additional treatment is needed. If your baby is born Rh positive, you’ll need another injection shortly after delivery.
If the antibody screen shows that you’re already producing antibodies, an injection of Rh immune globulin won’t help. Your baby will be carefully monitored. If necessary, he or she might be given a blood transfusion through the umbilical cord during pregnancy or immediately after delivery.
Mother’s Rh factor Father’s Rh factor Baby’s Rh factor Precautions
Rh positive Rh positive Rh positive None
Rh negative Rh negative Rh negative None
Rh positive Rh negative could be Rh + or Rh – None
Rh negative Rh positive could be Rh + or Rh – Rh immune globulin injections



cenforce 150 mg sildenafil sildenafil for ed dosage
stromectol online cost of ivermectin 1% cream
stromectol lotion buy ivermectin canada
how to make tadalafil tadalafil troche side effects
stromectol online stromectol buy uk
kmart pharmacy Diamox
value rx pharmacy irvine wal mart pharmacy canada
express rx pharmacy and medical supplies canadian pharmacy norco
erectile online pharmacy europe
Appreciate it. Ample forum posts.
expert essay writers what to write my college essay about write my paper for me free
With thanks! Lots of knowledge!
no deposit online casino win real money online casino atlantis casino online
With thanks. Wonderful information!
essay services customer service essay cheap essay service
Very good posts. Appreciate it.
nursing essay writing service [url=https://bestpaperwritingservice.com/]economic paper writing service[/url] pay to do my paper [url=https://bestonlinepaperwritingservices.com/]has anyone used a paper writing service[/url] writing service research paper sociology essay writing service [url=https://customthesiswritingservice.com/]best master thesis writing service[/url] good thesis sentences [url=https://writingthesistops.com/]thesis research[/url] thesis statement for animal farm